Have your say on the safety and quality of care provided in adult community-based mental health services.
Phoebe Averill
Twenty years have passed since the publication of a landmark report overseen by a former Chief Medical Officer for England, which kickstarted the patient safety movement in the UK.
The report, An organisation with a memory: Learning from adverse events in the NHS, drew attention to unacceptable failures in healthcare delivery, which at times had resulted in avoidable harm and distress to patients and their families.
A need for wholesale change in learning
The authors called for wholesale change in how the NHS learns from previous incidents, emphasising the importance of an open, honest culture where problems are discussed when something goes wrong.
They highlighted a need for a joined-up approach to reporting incidents so that services could reduce the chances of a mistake being repeated. Although poor quality healthcare has continued to make headlines due to a number of high-profile service failings, for example at Mid Staffordshire NHS Trust between 2005 and 2009, overall there has been huge progress in understanding and improving safety problems in many healthcare specialties.
However, mental health services have been left behind, with far fewer research studies focusing on safety in mental healthcare despite repeated safety failings.
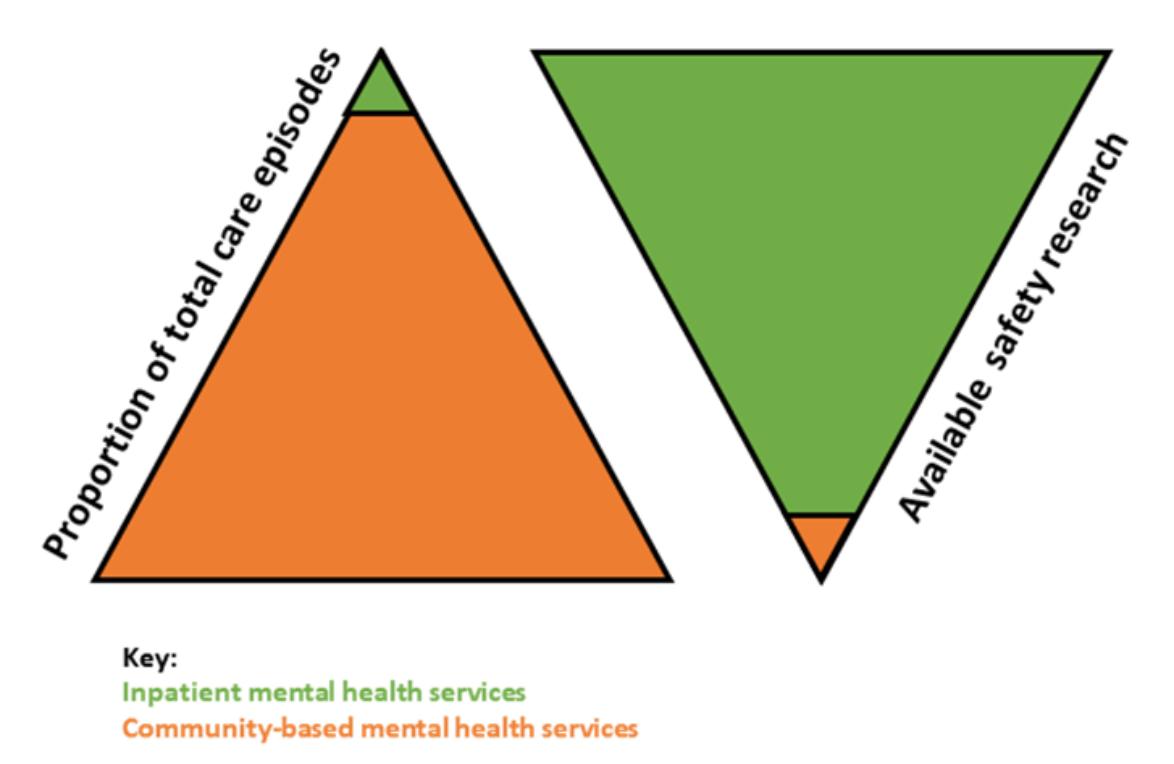
Efforts have been made to bring mental health services up to speed with other areas of healthcare, but almost all of the research and interventions focus on safety in acute inpatient mental health services. Very little is known about what ‘safe’ care looks like in community-based mental healthcare settings.
This matters because in the UK community-based mental health services vastly outnumber inpatient mental health services. In 2019, almost 98% of adult mental healthcare episodes took place in community settings. One size does not fit all, and it cannot be assumed that the same safety problems, causes, and solutions apply to community mental health services as to inpatient care.
Unique risks in outpatient care
People who access mental healthcare in outpatient settings may face unique risks to the safety of their care. These may include challenges associated with navigating multiple different care agencies, difficulty in accessing out-of-hours crisis support, receiving the wrong diagnosis, or physical health side effects of prescribed medications.
Several research studies point to the need to better understand safety in community-based mental health services. A study in the US compared safety events across different types of outpatient healthcare settings. Concerningly, incidents in mental health services were linked to greater levels of harm compared to other healthcare settings. In the UK, improving safety for mental health service users was identified as a top priority for future research into patient safety in primary care.
How can service users and carers help to improve mental healthcare?
The opinions and experiences of users of community mental healthcare and their family members and carers must be at the centre of future work to make care safer. Service users are experts in their own care.
Research in other areas of healthcare has shown that service users and carers play an important role in ensuring that care is safe, often noticing risks before healthcare professionals and helping to stop something going wrong. Worryingly, a study found that over three quarters of service users and carers found it difficult to raise concerns about the safety of mental healthcare.
It is important that the views of service users and carers are heard alongside those of healthcare professionals, so that the main risks to safety in community-based mental healthcare are understood and services can be improved.
Share your views about the safety of community mental health services
At King’s College London, we are carrying out a study to find out more about the safety and quality of care provided in adult community-based mental health services.
We would like to speak to service users, their families or carers, and people who deliver care in these settings to understand more about how safety could be improved and to hear about experiences of safe care in community mental health services.
If you are interested in finding out more information or taking part, please follow these links if you are a service user or carer or a healthcare professional.
Phoebe Averill is a PhD student at King’s College London focusing on improving the safety and quality of the mental healthcare that people receive.
